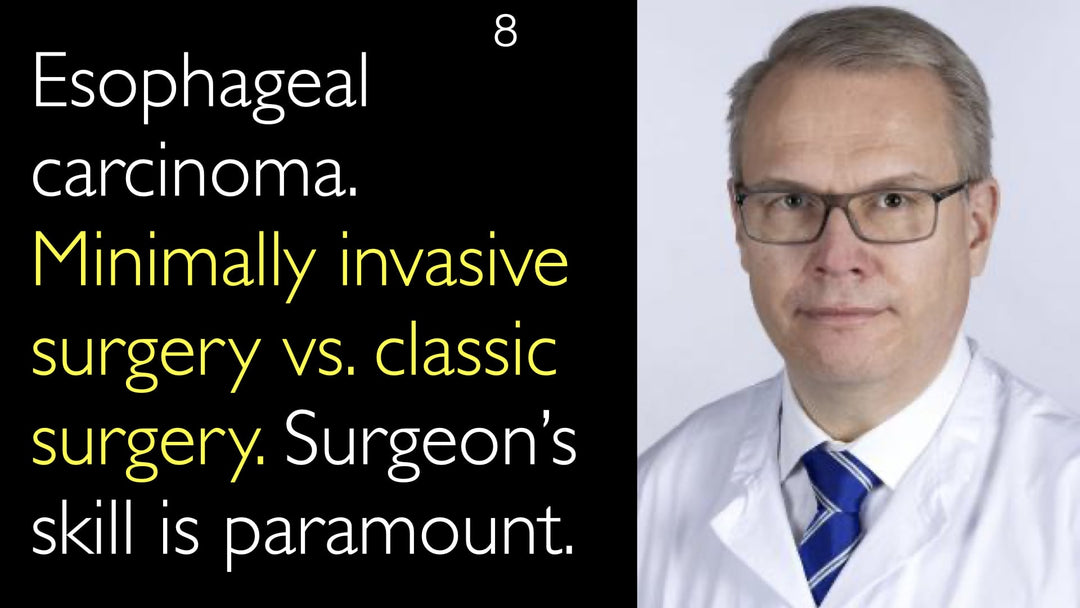
Leading expert in esophageal cancer surgery, Dr. Jari Rasanen, MD, explains how minimally invasive esophagectomy improves patient outcomes. He details the surgical techniques and compares them to classical open surgery. Dr. Jari Rasanen, MD, emphasizes that a surgeon's skill and experience are paramount for success. He discusses the significant reduction in pulmonary and cardiovascular complications with a minimally invasive approach. Long-term survival rates are similar, but quality of life is often better after minimally invasive surgery.
Minimally Invasive Esophagectomy: Techniques, Outcomes, and Surgeon Expertise
Jump To Section
- Surgical Treatment Efficacy
- Minimally Invasive Technique
- Patient Selection Criteria
- Surgeon Skill Importance
- Long-Term Outcomes Comparison
- Quality of Life Benefits
- Full Transcript
Surgical Treatment Efficacy in Esophageal Cancer
Dr. Jari Rasanen, MD, confirms that surgery remains the fundamental part of curative treatment for esophageal cancer. He states that a successful surgical outcome requires the procedure to be safe for the patient. In specialized centers, five-year survival rates after esophagectomy should exceed 50%. Dr. Jari Rasanen, MD, notes that advancements in chemotherapy and chemoradiation are important, but they complement rather than replace the role of surgery.
Defining the Minimally Invasive Technique
Minimally invasive esophagectomy replaces large incisions with small keyhole openings. Dr. Jari Rasanen, MD, explains that in the abdomen, a laparotomy is replaced by laparoscopy. In the chest, a large thoracotomy is replaced by thoracoscopy. This approach allows surgeons to perform the same oncological procedure as in open surgery. The technique is designed to achieve the same cancer removal goals with less physical trauma.
Patient Selection Criteria for Surgery Type
Dr. Jari Rasanen, MD, indicates that most esophageal cancer cases are suitable for a minimally invasive approach. The decision is not solely based on the patient's disease characteristics. The surgeon's comfort and expertise with the technique are critical factors in the decision-making process. The primary goal is always to perform the safest and most effective operation for the individual patient.
The Paramount Importance of Surgeon Skill
Dr. Rasanen strongly emphasizes that minimally invasive esophageal surgery is highly operator-dependent. A surgeon's experience is the most important factor in determining the best surgical approach. He advises that if a surgeon lacks extensive experience in minimally invasive techniques, performing an open esophagectomy is the safer option. This prioritizes patient safety and helps avoid preventable complications. Dr. Anton Titov, MD, and Dr. Rasanen agree that open surgery remains a completely viable and often preferable choice when aligned with the surgeon's skill set.
Comparing Long-Term Surgical Outcomes
Overall survival rates between open and minimally invasive esophagectomy appear to be very similar. Dr. Jari Rasanen, MD, references studies that sometimes show a slight survival advantage for the minimally invasive approach. However, he cautions that patient selection and other confounding factors can influence these results. The oncological efficacy, including local recurrence rates, is equivalent when the procedures are performed correctly.
Short-Term and Long-Term Quality of Life Benefits
The short-term benefits of minimally invasive esophagectomy are well-established and significant. Dr. Jari Rasanen, MD, highlights a major reduction in postoperative pulmonary complications. Patients also experience less pain and have shorter hospital stays after minimally invasive surgery. Cardiovascular complications are less frequent compared to open surgery. Dr. Jari Rasanen, MD, concludes that patients often do better both in the short and long term, with some studies showing superior long-term quality of life after a minimally invasive procedure.
Full Transcript
Dr. Anton Titov, MD: Efficacy of surgical treatment of cancer is one of your research interests. In outcome studies, how effective is surgical treatment for esophageal cancer? How can it be improved further?
Dr. Jari Rasanen, MD: Although there have been many developments in chemotherapy and chemoradiation therapy, I think that most surgeons and doctors agree that surgery is still the fundamental part of curative treatment for esophageal cancer. Of course, the surgery must be safe for the patient.
One of the things we have been doing in our institution to make it safe is using minimally invasive esophageal surgery since 2009. By that, we have reduced the number of complications, especially pulmonary complications. This makes the surgery safe for the patient.
On the other hand, results in good surgical centers should show at least more than 50% five-year survival after surgery if you are a specialized center.
Dr. Anton Titov, MD: Professor Rasanen, what is minimally invasive esophageal cancer surgery? How does it differ from the classical approach? How do you decide if a patient merits minimally invasive surgery versus a classical approach in esophageal cancer?
Dr. Jari Rasanen, MD: Minimally invasive surgery in esophageal surgery means the same thing as in all surgery. You are replacing the big incision laparotomy by laparoscopy in the abdomen. Then in the chest, you are replacing a large thoracotomy by thoracoscopy.
You make only small keyholes, and you can do the same thing as in open surgery through those holes. So basically, most esophageal cancer cases are suitable for minimally invasive surgery.
It depends on the surgeon's experience whether he can perform the minimally invasive procedure or if he is doing the open esophagectomy better. This is very important to note: minimally invasive approaches in esophageal surgery and lung cancer surgery are very operator-dependent.
Perhaps for some patients, it's better to do the surgery with a classical approach if the surgeon is not very experienced and skillful with minimally invasive surgery.
Dr. Anton Titov, MD: Exactly, it very much depends on the experience of the surgeon. I completely agree that if the surgeon doesn't have much experience in minimally invasive surgery, it is a better option to do open surgery and avoid complications that can occur during minimally invasive surgery due to lack of experience. So basically, I still think open surgery is a viable option if the surgeon feels more comfortable with open surgery.
Dr. Anton Titov, MD: What do long-term results look like when you compare minimally invasive approaches for esophageal cancer and the more classical approach? Are the local recurrence rates the same? Do they differ? What about the long-term quality of life of patients? Short-term outcome is much better with minimally invasive esophageal surgery, we know that. But what about the long-term outcomes?
Dr. Jari Rasanen, MD: The overall survival seems to be pretty much the same after open and minimally invasive surgery. Some studies show that overall survival can be a little better after minimally invasive surgery than after open surgery, both in esophageal and lung surgery. But it is very difficult to say whether it depends on patient selection or other confounding factors.
Therefore, I think the main thing is that quality of life, especially in the short term, is better for the patient after minimally invasive surgery. Some studies show that long-term quality of life is also better after minimally invasive surgery.
Patients suffer significantly less from pain and have to stay a shorter time in the hospital. They also have fewer cardiovascular complications after minimally invasive surgery. So patients are doing a lot better after minimally invasive surgery, both in the short and long term.